What Is Depression?
CBT for Depression helps explain why sadness and clinical depression are not the same. Most people feel sad sometimes—but depression is different. It’s a medical condition where your brain gets stuck; it’s not a choice, weakness, or something you can “just think away.” In depression, brain chemistry, neural connections, and thought patterns shift in ways that create persistent hopelessness, emptiness, and loss of joy.
Common symptoms
- Persistent emptiness (emotional numbness)
- Loss of interest in activities once enjoyed (anhedonia)
- Physical exhaustion that doesn’t improve with rest
- Changes in sleep and appetite (too much or too little)
- Difficulty concentrating or making decisions
- Feelings of worthlessness or excessive self-blame
- Thoughts about death or suicide
The critical distinction: these feelings persist for at least two weeks straight (for a diagnosis), don’t improve with distraction or willpower, and significantly interfere with daily life—work, relationships, self-care.
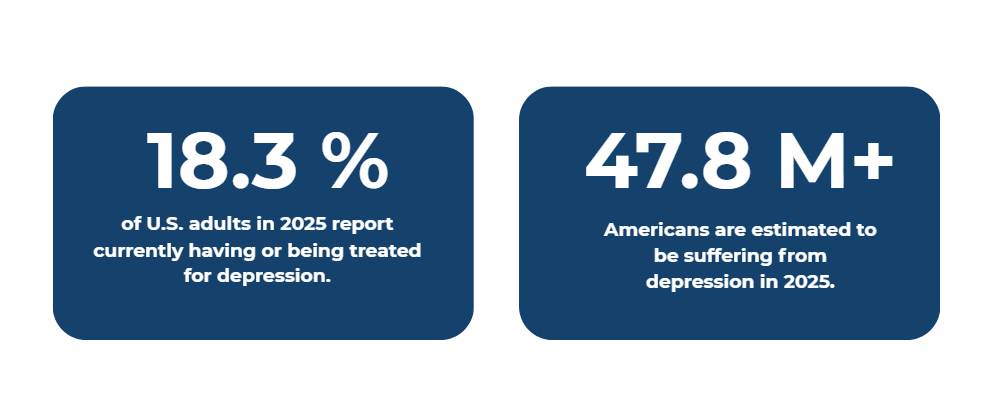
The Scale of Depression
The Brain Biology of Depression: What’s Actually Happening
To understand CBT for depression, we first need to understand what depression actually is at the neurological level. Depression isn’t simply a lack of willpower—it’s a dysregulation of the brain systems that control mood, motivation, reward, and emotional processing.
The Neurotransmitter Connection:
Your brain communicates through chemical messengers called neurotransmitters. In depression, three key neurotransmitters become dysregulated:

When depression develops, these neurotransmitter systems don’t work in isolation—they interact with stress hormones, genetic factors, and life experiences to create a complex dysregulation. People with clinical depression often have increased levels of an enzyme called MAO-A that breaks down these neurotransmitters, resulting in very low levels of serotonin, dopamine, and norepinephrine.
The Brain Regions Affected
Depression doesn’t just affect neurotransmitter levels—it changes the structure and function of specific brain regions:
- The Amygdala (emotion center): Becomes overactive, making your brain hypersensitive to negative information. Everything gets processed through a “threat filter.”
- The Prefrontal Cortex (rational thinking): Becomes underactive, reducing your ability to challenge negative thoughts or make rational decisions.
- The Hippocampus (memory and learning): Can shrink under chronic stress, making it harder to remember positive experiences or learn new patterns.
- The Limbic System (emotion regulation): Shows reduced connectivity with the thinking brain, making emotions feel overwhelming and impossible to regulate.

How the Depression Cycle Traps You (And Why Escape Feels Impossible)
Understanding the depression cycle is crucial because CBT targets exactly these points of entrapment. Depression doesn’t just sit there passively—it actively maintains itself through a vicious loop.
- Negative thoughts (“I’m worthless”)
- Depressed mood (hopelessness)
- Avoidance (withdrawal, canceling plans)
- Worsening symptoms (isolation, fewer positive experiences)
Here’s how this cycle works in real life:
Step 1 – Negative Thoughts: Your brain generates thoughts like “I’m a failure,” “Nobody cares about me,” or “Things will never get better.” These aren’t random—they emerge from the dysregulated limbic system and underactive prefrontal cortex.
Step 2 – Emotional Consequence: These thoughts trigger depressed mood, despair, and emptiness. The mood feels like absolute truth—like proof that the thoughts are correct.
Step 3 – Behavioral Response: You withdraw. You cancel plans. You stay in bed. You avoid people, work, and activities. This feels protective in the moment—like you’re protecting yourself from disappointment.
Step 4 – The Trap Tightens: The avoidance actually makes everything worse. You lose connection to people who care. You don’t accomplish anything (confirming “I’m a failure”). Your brain doesn’t get the positive experiences it needs to restore neurotransmitter balance. The cycle strengthens.
This is why depression feels so permanent and why “just think positive” doesn’t work—the brain’s structure, chemistry, and thought patterns are all reinforcing each other. Every withdrawn day, every avoided social interaction, every negative thought trains your brain deeper into the depression pattern.
How CBT Breaks the Cycle Of Depression
CBT is powerful because it doesn’t try to fix just one part of the depression cycle—it interrupts the cycle at multiple points simultaneously. The remarkable aspect of CBT is that when you change your thoughts and behaviors, you physically change your brain’s structure. Neuroplasticity means your brain can adapt and rewire itself.

When you work to adopt different ways of thinking and behaving through CBT, your brain responds by adapting to those new thoughts and behaviors. The amygdala becomes less reactive, the prefrontal cortex strengthens, and new neural connections form.
Four Core CBT Techniques That Actually Work
1) Behavioral Activation — Movement Creates Mood Change
Act first; mood follows. Schedule small, meaningful actions (15-minute walk, text a friend, one task). Do them without waiting for motivation; note mood shifts after. Action triggers dopamine and restarts reward circuits.
2) Cognitive Restructuring — Challenge the Depression Lies
Spot distortions (all-or-nothing, catastrophizing, mind-reading, personalization, overgeneralization). Ask: What’s the evidence for/against? What would I tell a friend? What’s a balanced view? Repeated practice strengthens cognitive control regions.
3) Activity Scheduling — Structure Replaces Chaos
Plan the week (sleep/wake, meals, work/study, movement, social contact, one enjoyable activity daily). Treat items like appointments. This reduces decision fatigue, builds accomplishment, and creates accountability.
4) Behavioral Experiments — Test Predictions
Write the prediction (“People will think I’m awkward”), do the activity anyway, observe outcomes. Reality usually disproves depressive forecasts, weakening them over time.
Why Online Therapy Changes Everything for Depression
Here’s a painful truth: When you’re depressed, the hardest thing in the world is leaving your house. The fatigue, the shame, the overwhelm—they all make getting to an office feel impossible.
Online therapy removes this barrier completely. You can receive evidence-based CBT from your bed, your couch, or anywhere safe. Research shows that therapist-guided online CBT works just as well as in-person—but with massive advantages when depression is involved.
Why online CBT is particularly powerful for depression:
- Removes access barriers: No commute, no need to leave home, no excuses to cancel
- Provides comfort: You can be in your safe space while doing vulnerable work
- Increases privacy: Greater comfort sharing difficult feelings when fully private
- Enables homework monitoring: Your therapist can check in on assignments between sessions via secure messaging
- Creates accountability: Digital check-ins and reminders help with follow-through when motivation is low
- Maintains consistency: You’re less likely to cancel video sessions than drive to an office
Key advantage: External accountability keeps you engaged when motivation is scarce.
Getting Started: Your Path Forward
If depression has taken months or years from you—and thinking your way out hasn’t worked—the evidence is clear: CBT works, and you don’t have to do this alone. The most important step is the first one.

Resources for Support and Recovery
- Mayo Clinic: Offers comprehensive information on depression, its symptoms, and treatment options.
- National Institute of Mental Health (NIMH): Provides resources and research on mental health disorders, including depression.
- American Psychological Association (APA): Features articles on the benefits of therapy, mindfulness, and self-care practices for mental health.
- Psychology Today: Includes expert insights on managing depression and finding purpose in life.
By utilizing these resources and embracing natural depression relief strategies, you can take meaningful steps toward a life filled with hope and happiness.
Crisis Support: If you’re having thoughts of self-harm or suicide, contact the 988 Suicide & Crisis Lifeline (call or text 988) or go to the nearest emergency room. You deserve immediate support.


